VITAMIN-D
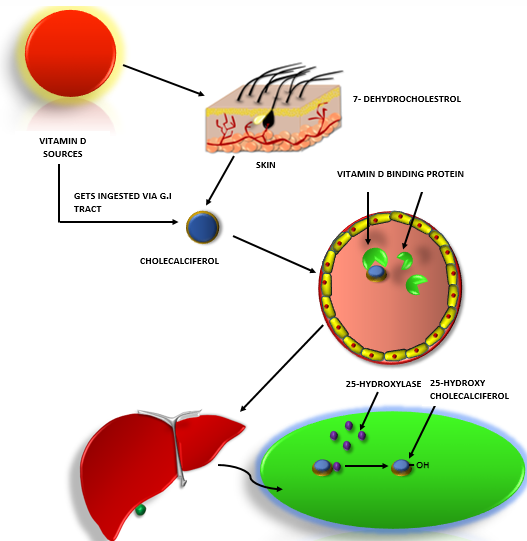
Vitamin-D is fat soluble steroid hormone which can be obtained from the sources such as yoghurt, liver, egg yolk, cereals, mushrooms, milk, etc. The Vitamin-D gets absorbed through the food source ingested in gastrointestinal tract and skin. Vitamin-D has the ability to form micelles when get bound to the fat cholesterol.

VITAMIN-D PATHWAY:
In the skin when light is absorbed, 7- Dehydrocholestrol the precursor for vitamin-D gets converted to cholecalciferol. And in the gastrointestinal tract, vitamin D adhere to fat cholesterols converting into cholecalciferol and moves into the gut.
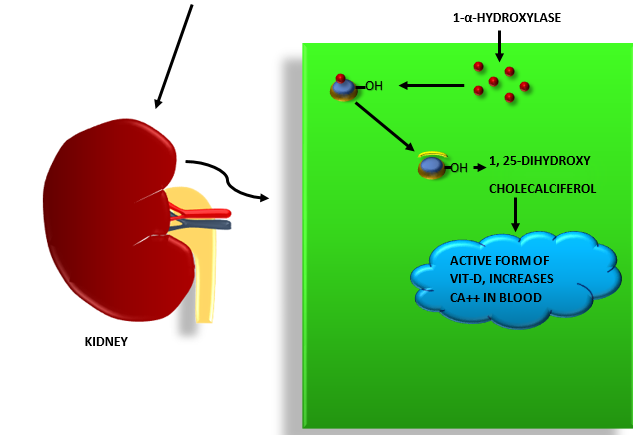
For the movement of the vitamin D across the blood stream, the cholecalciferol has to get bound to specific binding proteins called Vitamin D Binding proteins. Vitamin D travels from the bloodstream to the liver which has an enzyme known as 25- Hydroxylase. 25- Hydroxylase catalyzes the conversion of cholecalciferol into 25- Hydroxycholecalciferol by adding a hydroxyl group on 25th carbon of cholecalciferol. The 25- Hydroxycholecalciferol travels into the proximal convoluted tubules of kidney. The 1-α-Hydroxylase enzyme which is present in kidney, catalyzes the formation of active form of vitamin D known as 1, 25- Dihydroxycholecalciferol from 25-Hydroxycholecalciferol by adding a hydroxyl group on the 1st carbon of cholecalciferol.
WHAT IS THE ROLE OF IMMUNE CELLS IN RELATION TO THE VITAMIN D?
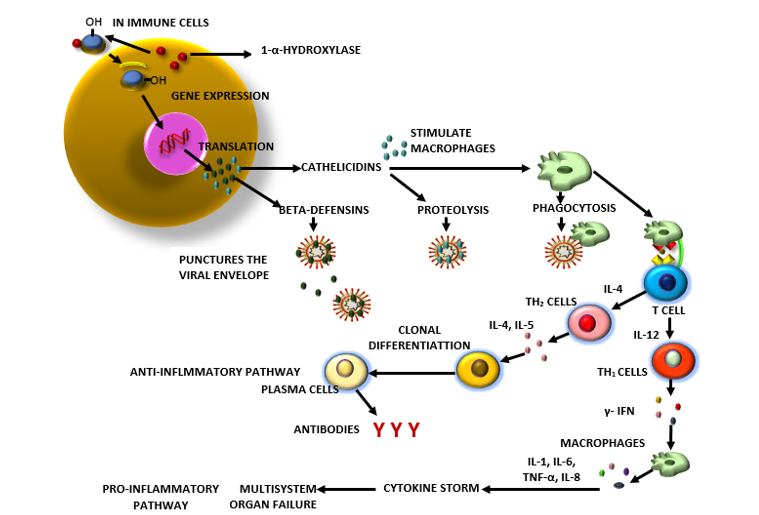
- Even the immune cells have the enzyme 1-α-Hydroxylase, which helps for the formation of the active Vitamin D i.e. 1, 25-Dihydroxycholecalciferol from 25-hydroxycholecalciferol.
- The vitamin D binds to the vitamin D receptors present in the immune cells and are taken into the nucleus activating a specific gene. This gene undergoes transcription process to produce mRNA which codes for different proteins called cathelicidins and beta defensins. The cathelicidins and beta defensins are antimicrobial proteins
- In some research studies, beta defensins is shown to have defense mechanism against respiratory syncytial virus, rhinovirus and influenza virus. The beta defensins plays a role in forming holes into the viral envelope. Thus increasing the expression of Beta defensins will lead to destruction of viruses.
- Cathelicidins acts on the virus by cleaving the viral proteins through proteolysis and leading to the destruction of virus.
- Cathelicidins have the ability to stimulate the macrophages and can also increase the vascular permeability where the pathogen is residing.
- Cathelicidins guides the macrophages to move to the site where the pathogen is through chemotaxis.
- Activated macrophages engulfs the virus particles through a process known as phagocytosis.
- The viral particles are presented by the macrophages to the T cells. As the viral particle is new to the T cell, it is known as Naïve T cell.
- This naïve T cell are stimulated by the IL-4 to become Th2 cell (type of T helper cell) which releases more cytokines like IL-4 and IL-5. These interleukins activates B-lymphocytes.
- B cells undergoes clonal proliferation into plasma cells. Those plasma cells produces antibodies specific to the antigen that are presented by the macrophages. In SARS-CoV2, the antigen molecules are the S peptides.
- The antibody-antigen binding enhances the complement system, increases the phagocytosis or neutralizes the virus.
- This pathway, where the Th2 cells are activated is known as Anti-inflammatory pathway.
- The naïve T cells undergoes another pathway known as pro-inflammatory pathway when these naïve cells are not activated into Th2 cells. This pathway influences body in the negative way and may lead to many complications in the body.
- When Th2 cells are activated, it plays a major role in inhibiting the pro-inflammatory pathway.
- In pro-inflammatory pathway, the naïve T cells releases Il-12 to activate Th1 cells which then releases γ-IFN.
- The γ-IFN activates the macrophages which releases the cytokines. Thus increased levels of IL-1, TNF-α, IL-6, IL-8 and chemokine’s are seen.
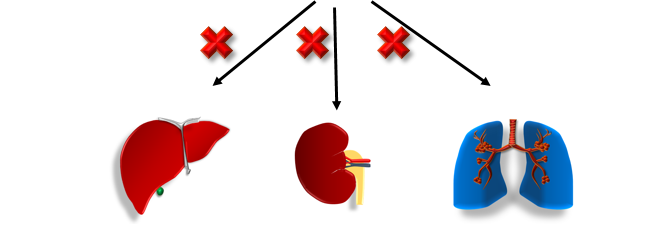
- The increased levels of cytokines causes massive inflammation which leads to cytokine storm in the body. The increased cytokine levels in the body acts on different organs causing multiple organ failure.
- In the liver, increased cytokines triggers the production of Acute Phase reactive proteins like CRP, fibrinogen, ferritin.
- The kidneys are effected by acute kidney injury. The lungs are affected by Acute Respiratory Distress Syndrome (ARDS).
- The increased cytokines even effects the heart by causing myocardial infarction and heart failure.
- The increased CRP levels causes inflammation on blood vessels and thus increases the risk of thrombosis.
- Thus patients with coronary artery disease, diabetes mellitus, hypertension will have more risk towards the increased risk of getting infected with serve COVID-19 and may increase the complications.
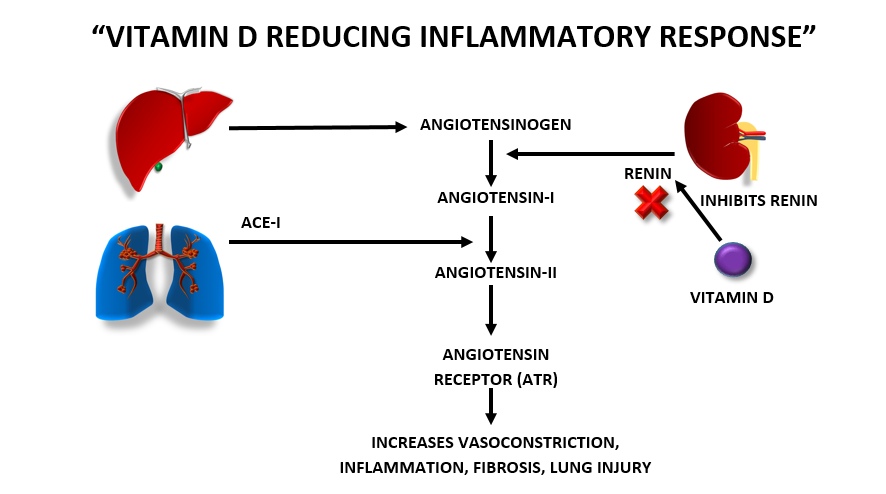
“VITAMIN D PLAYS A MAJOR ROLE IN REDUCING THE INFLAMMATORY RESPONSE”
- In the liver, Angiotensinogen is produced which gets converted into Angiotensin Type -I (AT-I) which is stimulated by renin present in kidney.
- The ACE-I (Angiotensin Converting Enzyme-I) present in lungs stimulates the conversion of AT-I to AT-II. The increased levels of AT-II increases lung injury.
- High levels of AT-II binds to Angiotensin Receptor (ATR), thus increasing vasoconstriction, inflammation and fibrosis leading to lung injury.
- Vitamin-D inhibits this pathway by inhibiting the renin, thus renin will not be able to stimulate downstream conversions. This prevents lung injury.
- Vitamin- D can even stabilize the cell membrane of pulmonary capillaries endothelium.
- The ACE-II stimulates conversion of AT-II to AT-(1-7) which decreases inflammation, fibrosis and increases vasodilation, thus preventing lung injury.
- In COVID-19 patients, the SARS CoV2 attacks the ACE-II. As levels of ACE-II are decreased, the patients have increased risk of lung injury.
- As per the research studies, Vitamin D can stimulate and enhance the activity of ACE-II. More of the research studies are to be done on the area for more specific results.