Covid-19 (SARS-CoV-2) severe acute respiratory syndrome coronavirus 2, novel and contagious pneumonia, similar to SARS Coronavirus.
Dawn of pandemic:
The transmission of the virus to the humans were observed to the people of Wuhan, Hubei province In China. It is likely said to be originated from bats and eventually transmitted by unknown carriers to the human.
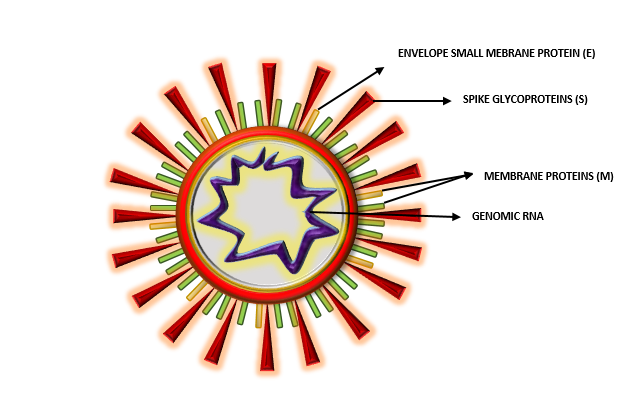
Structure:
On the structural basis, the spike (S) proteins of the virus are the potential cause for the viral attachment and entry and also an important factor for their pathogenicity. Studies have reported the Homo-trimer structure of spike glycoprotein, and discovered the S1 domain of Covid 19 spike glycoprotein, which defines their virulence and hijacks the immunoregulatory factor interacting with the human CD26. The viral outer membrane spike proteins are the primary site for glycosylation. These are crucial for the cell adhesion, adhering the host cells such as CD26, AC2, Ezrin, cyclophilins). To determine the structure of the virus, scientists have used cryo-electron microscopy imaging the structure of RNA- Dependent RNA polymerase nsp12. nsp 12 with other two cofactors nsp 7and nsp 8, involves in a process to synthesize the viral RNA. It bears a β-hairpin domain at its N-terminus. The viral structure provides a basis for designing and development of new antiviral therapeutics. Results from ClUSTAL- W sequences alignment of COVID-19 and SARS-CoV spike glycoproteins have shown differences in three regions and 91% similarity in S2 Domain region. The S1 domain was found to have the sequence differences, which a important structure for cell adhesion and virulence. Researchers predicted N- and O- glycosylation sites on the surface of the viral glycoproteins. Glycosylation patterns were used to study the differences between shielded structures of COVID-19 and SARS- CoV spike glycoproteins. COVID-19 showed some of the unique glycosylation sites compared to SARS-CoV suggesting difference in shielding or glycan camouflage patterns of spike proteins, which harms the host immunity.
PATHOPHYSIOLOGY OF COVID19:
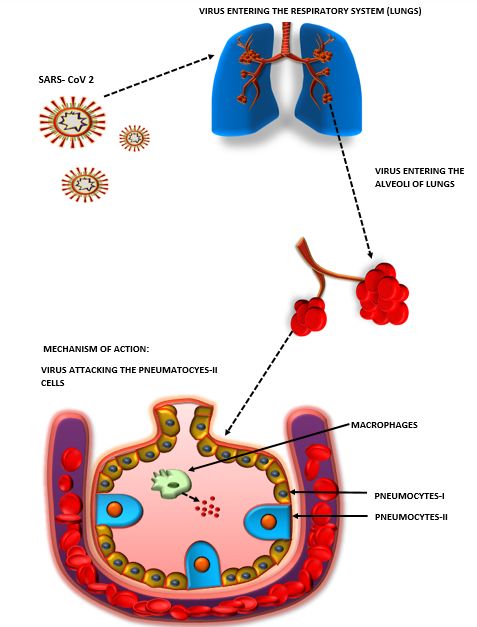
- An individual comes in contact with the viral particles via different medium of contact and the major route of entry of the respiratory droplets is when an infected individual coughs or sneezes. It can even spread out from the faecal matters.
- The viral particles in respiratory droplets sustains for 3 hours and survives on any surface for about 24 hours.
- The viral particles enters through the nasopharyngeal route invading the lungs.
- The virus attacks the alveoli and damages the pneumocytes- II cells of the alveoli.
- There are two types of cells present in the alveoli: pneumocytes-I and pneumocytes-II. The pneumocyte-I plays a role in gaseous exchange and pneumocytes-II produces surfactants which decreases the surface tension within the alveoli and thus reduces collapsing of alveoli.
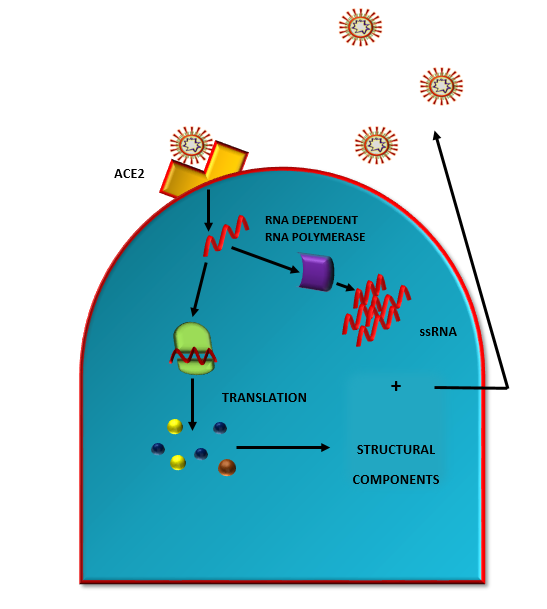
- The spike proteins of the virus binds to the cell surface receptors of pneumocytes—I called ACE2 (Angiotensin Converting Enzyme-2).
- The positive sense single stranded RNA is released into the cell. After arriving into the cell, it uses the host ribosome to undergo translation to produce proteins. It produces a group of different proteins.
- This different group of proteins are used for making all the protein components of the virus such as capsid, spike proteins, etc.
- After translation, the proteins produced are proteolyzed by proteinases to give components of the virus structure.
- Even this ssRNA has the ability to use RNA dependent RNA polymerase. Thus more of the ssRNA are produced using the enzyme RNA polymerase.
- These copies of ssRNA are incorporated into the structural components of the virus, thus as a results many copies of the virus are generated in the cell.
- At this stage, the pneumocytes-II cells are damaged which in response to the inflammation caused releases inflammatory mediators.
- These inflammatory mediators stimulates the macrophages. The macrophages then secrets cytokines like IL-1, IL-6, TNF-α.
- Dilation of the endothelial cells are caused when these cytokines passes to the blood stream. Thus endothelial cells undergoes contraction.
- The dilation results in various consequences like vasodilation and increased capillary permeability.
- Due to which fluids or plasma starts to leak in the interspatial spaces and accumulates in alveoli.
- The accumulation leads to compression of alveoli. The fluids entering into alveoli causes alveolar edema which is due to the decrease in the surfactant produced by the pneumocytes-II cells.
- As a result the surface tension in alveoli increases leading to alveolar collapse.
- Alveolar collapse decreases the gas exchange efficiency causing hypoxemia which increases the rate of breathing in patients.
- As a response to inflammation, the inflammatory mediators brings neutrophils to the site of damage.
- For the destruction of the virus, the neutrophils releases reactive oxygen species (ROS) and proteases.
- As neutrophils constantly releases the ROS and proteases, it unwantedly ends up in damaging the alveolar cells.
- The damaged alveoli will be accumulated with cell debris, fluids, etc. altering the gas exchange process leading to hypoxemia. This contributes to alveolar collapse.
- This process will cause constantly coughing.
- The cytokines travels to the central nervous system via blood, stimulating hypothalamus to release prostaglandins.
- These prostaglandins elevates the body temperature causing Fever.
- In this condition, usually the partial pressure of oxygen lowers in the body. In response to low oxygen levels, chemoreceptors are stimulated, triggering a reflux which causes sympathetic nervous system to get stimulate and increase the patient’s heart rate thus increasing respiration rate.
- Inflammation in lungs leads to systemic inflammatory response syndrome which results in septic shock.
- As a result, the decrease in blood volume and total peripheral resistance is seen. Thus patient blood pressure decreases leading to hypotension.
- This decreases the perfusion to multiple organs in the body leading to multiple organ failure.
- The ability of the kidney’s to get rid of creatinine and blood urine nitrogen decreases because of decreased blood flow.
- The elevated levels of creatinine and blood urine nitrogen are observed in the samples of patient’s blood sample.
- It also impacts the liver, the liver releases inflammatory enzymes such as AST, BILI, ALT and Acute phase reactants such as CRP, Fibrinogen, IL-6. This all enzymes are seen to be present in high levels.
- This all symptoms gives a major impact on the body, which eventually leads to mortality.
IMMUNOPATHOLOGY:
The COVID- 19 symptoms are detected to be in the range of mild to moderate, whereas 15 % of individuals exhibit severe symptoms resulting into severe pneumonia and later may develop Acute Respiratory Distress Syndrome (ARDS) leading to septic shock and/or multiple organ failure. The infected individuals are provided with the clinical treatment with ventilators and oxygen therapy. The virus triggers innate as well as adaptive immunity activating the host’s immune inflammatory responses and known to damage the host’s immune system. Thus, impaired immune system leads to harmful tissue damage. “Lymphopenia”, is the common feature of COVID-19 patients, especially individuals dealing with serve symptoms, CD4+ T cells, CD8+ T cells, B cells and natural killer (NK) cells and even the percentage of monocytes, eosinophil’s and basophils are drastically reduced in the body. The best way to get prevented from the virus is to get vaccinated as early as possible.